As stroke severity tool for large vessel occlusion takes center stage, this opening passage beckons readers into a world crafted with good knowledge, ensuring a reading experience that is both absorbing and distinctly original.
Stroke severity tool for large vessel occlusion plays a crucial role in clinical practice, aiding in the assessment of stroke severity and guiding treatment decisions. This comprehensive guide delves into the development, validation, and clinical applications of stroke severity tools, with a specific focus on large vessel occlusion.
1. Introduction
Stroke is a devastating neurological disorder that occurs when blood flow to the brain is interrupted, leading to brain damage and a range of functional impairments. The severity of a stroke can vary greatly, from mild deficits that resolve quickly to severe disability or even death.
Accurately assessing stroke severity is crucial for guiding treatment decisions and predicting patient outcomes.
2. Overview of Stroke Severity Tools
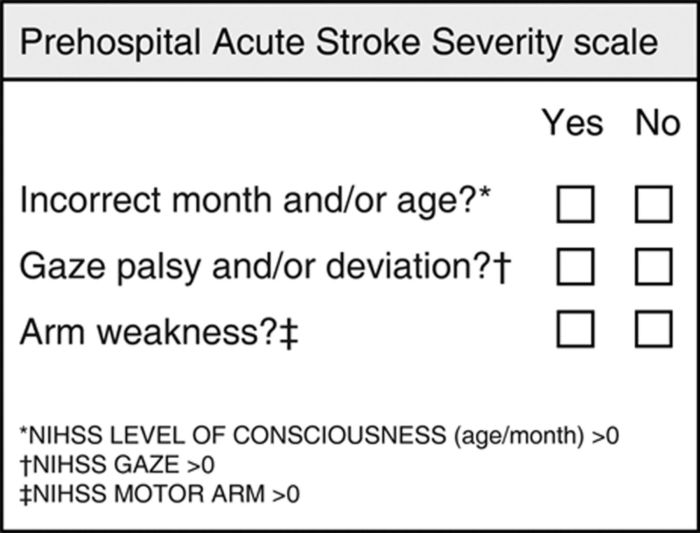
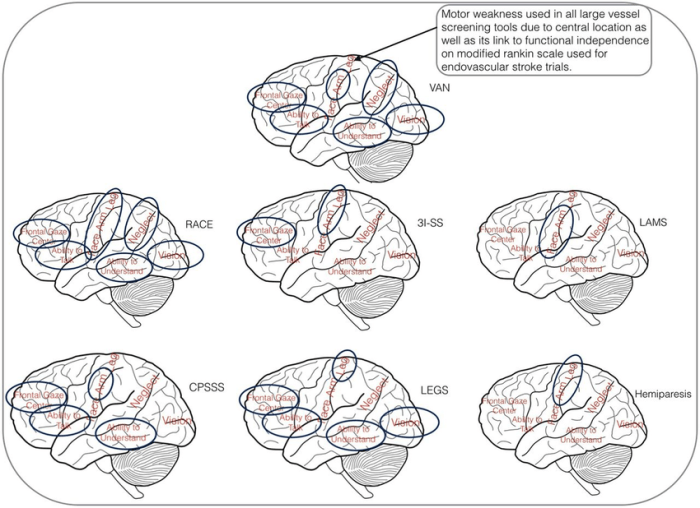
Stroke severity tools are standardized assessment methods used to quantify the neurological deficits and functional limitations caused by a stroke. These tools can be categorized into clinical scales and imaging techniques.
Clinical Scales
- National Institutes of Health Stroke Scale (NIHSS): A comprehensive scale that assesses various aspects of neurological function, including consciousness, language, motor function, and coordination.
- Modified Rankin Scale (mRS): A simple scale that assesses overall functional status and disability levels.
Imaging Techniques, Stroke severity tool for large vessel occlusion
- Computed tomography (CT) and magnetic resonance imaging (MRI): These imaging techniques provide detailed anatomical information about the brain and can help identify the location and extent of stroke damage.
- Perfusion imaging: This advanced imaging technique measures blood flow to different brain regions and can help identify areas of ischemic penumbra, which are potentially salvageable tissue.
Each stroke severity tool has its own advantages and limitations. Clinical scales are relatively simple to administer and can be used at the bedside, but they rely on subjective assessments and may not capture all aspects of stroke severity. Imaging techniques provide more objective and detailed information, but they can be more expensive and time-consuming.
3. Development and Validation of Stroke Severity Tools: Stroke Severity Tool For Large Vessel Occlusion
Developing and validating stroke severity tools is a rigorous process that involves several steps:
- Defining the target population and clinical outcomes of interest.
- Creating a pool of potential items or variables to assess stroke severity.
- Administering the tool to a large, representative cohort of patients with stroke.
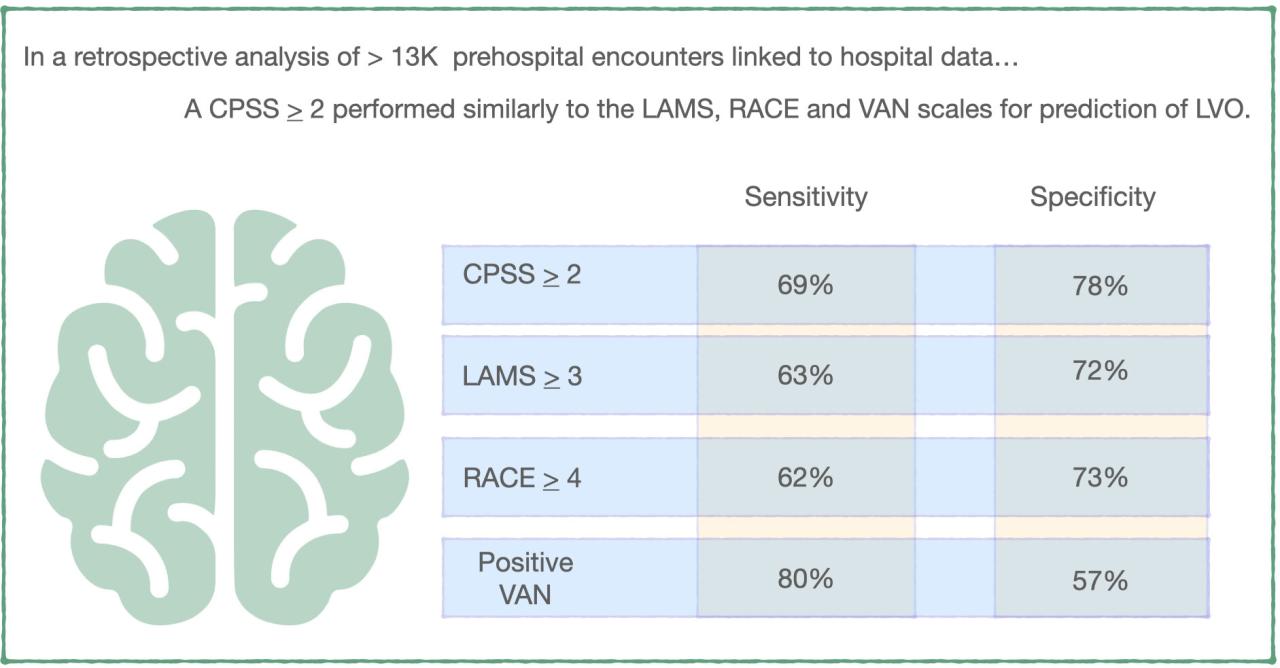
- Using statistical methods to evaluate the accuracy and reliability of the tool, including its sensitivity, specificity, and inter-rater reliability.
The validation process typically involves comparing the tool’s performance to other established stroke severity measures or to clinical outcomes, such as functional status or mortality.
Answers to Common Questions
What is the significance of assessing stroke severity?
Assessing stroke severity is crucial for guiding treatment decisions and predicting patient outcomes. It helps clinicians determine the appropriate level of care and intervention, such as thrombolysis or endovascular therapy.
How are stroke severity tools developed and validated?
Stroke severity tools are developed using large, representative patient cohorts and rigorous statistical methods. Researchers evaluate the accuracy, reliability, and predictive value of these tools to ensure their effectiveness in clinical practice.
What is the role of stroke severity tools in large vessel occlusion?
Stroke severity tools specifically designed for large vessel occlusion help clinicians assess the severity of stroke and determine the appropriate treatment approach. These tools consider factors such as the size and location of the occlusion, as well as the patient’s clinical presentation.